January 17, 2026
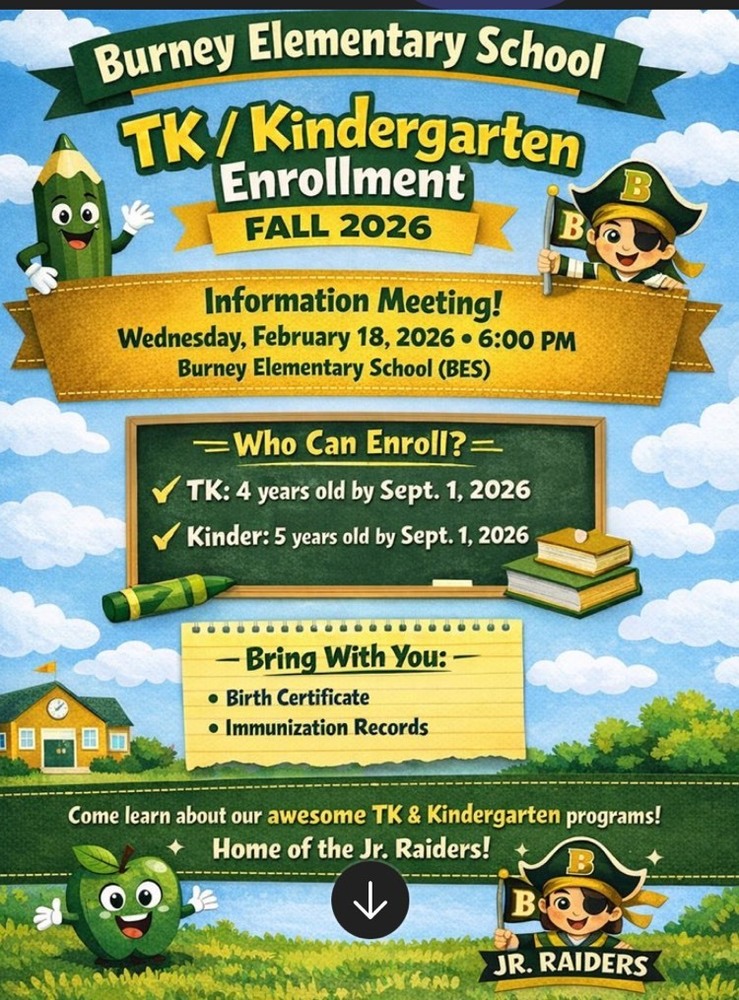
TK/Kinder Enrollment Meeting for Fall 2026! Information Meeting: Wednesday, February 18, 2026 6:00 PM at Burney Elementary School (BES). **If your child is currently enrolled i...

January 8, 2026
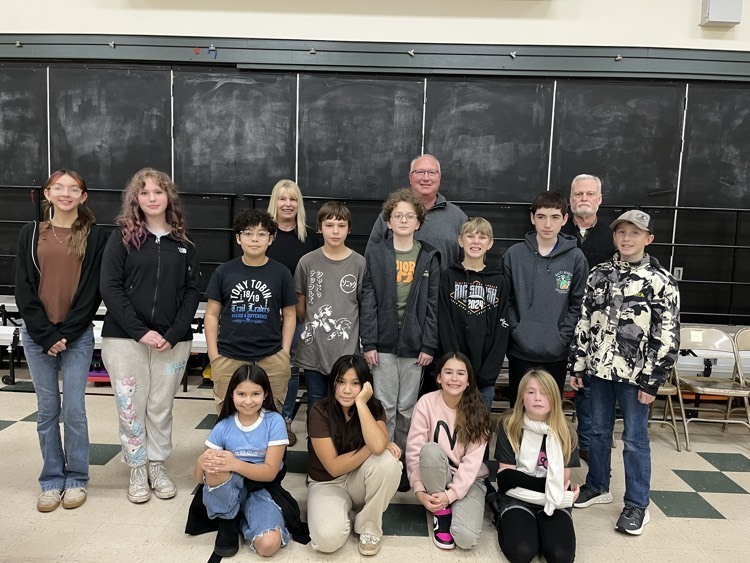
Spelling Bee 2025 We are so proud of all of our participants! Congratulations to Odin (3rd place), Jaxson (2nd place), and Tricia who will represent BES at the County Spelling...
November 16, 2025
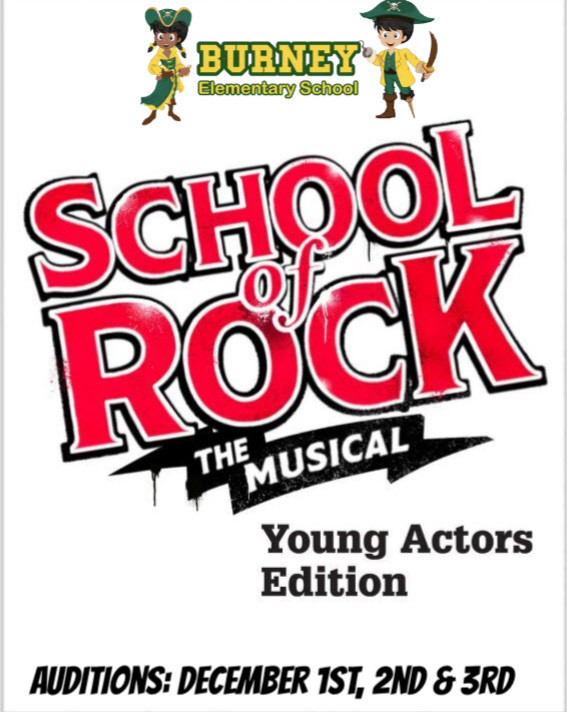
Spring Musical Auditions~ https://www.wejoinin.com/sheets/ukmfh
November 2, 2025
Burney Elementary honors National Native American Heritage Month by integrating Native American culture our the school community. The school employs a full-time Native Education pa...

October 30, 2025
Jr. Raiders in the news! Thank you KRCR. Check it out ~ https://drive.google.com/file/d/1u1m8zv6S7OBWISLWyD8vSxgfz09OV0mp/view?usp=drivesdk
October 25, 2025
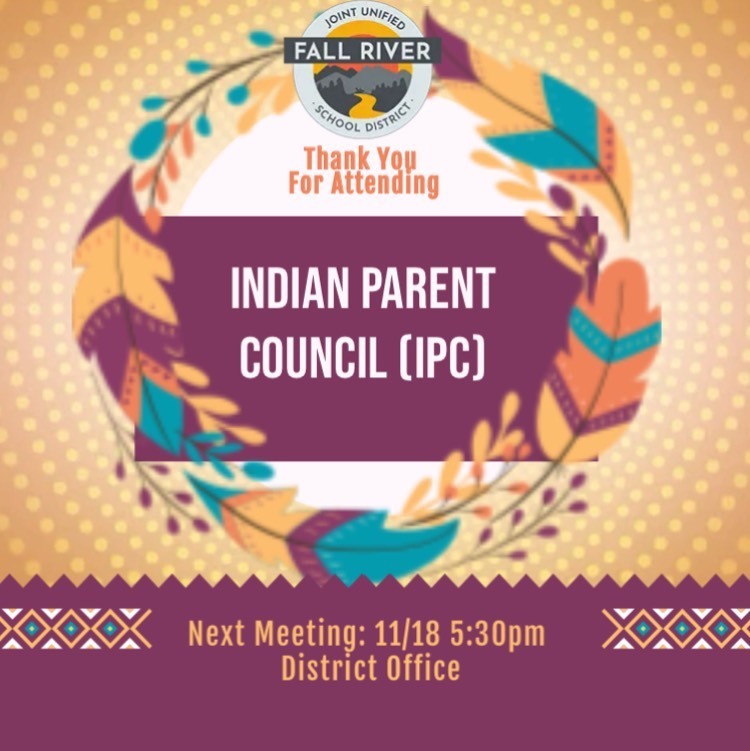
Indian Parent Council (IPC) Thank you and Congratulations to our newly elected officers: Chairperson: Juana Avila Vice Chair: Makayla Hinze Secretary: Tauni Orcutt High Sc...
October 17, 2025
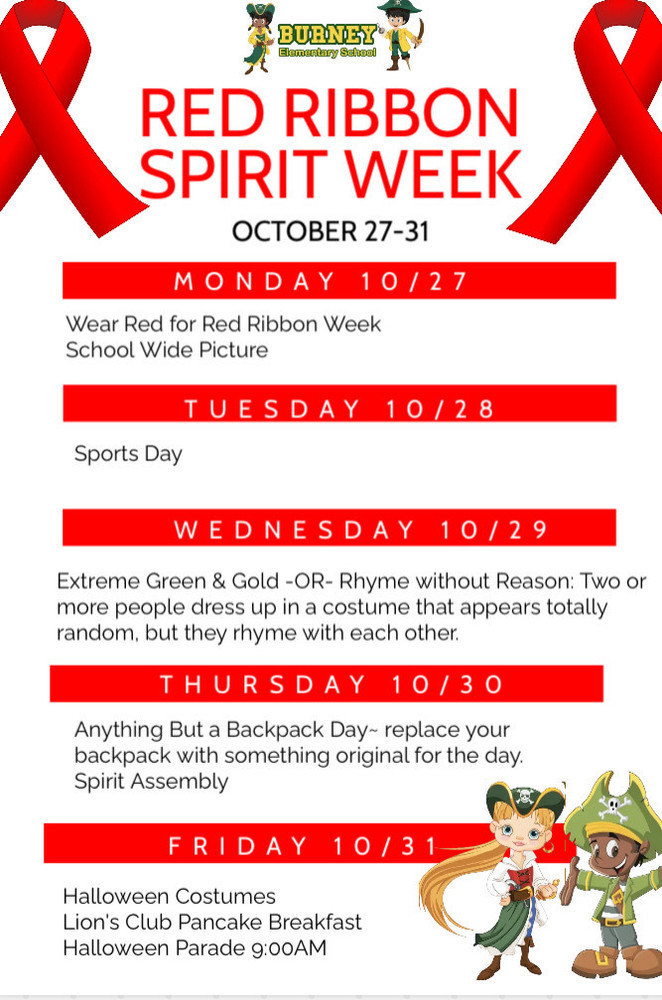
It’s almost time for Red Ribbon Week and Halloween Week at Burney Elementary! From October 27 to 31, we’ll join students across the nation in celebrating Red Ribbon Week—a time to...

October 10, 2025
🎄 Christmas Giving Project –Burney Elementary 🎄 We just learned there will be no Toys for Tots program in Shasta County this year. Many local families depend on that support t...
October 1, 2025
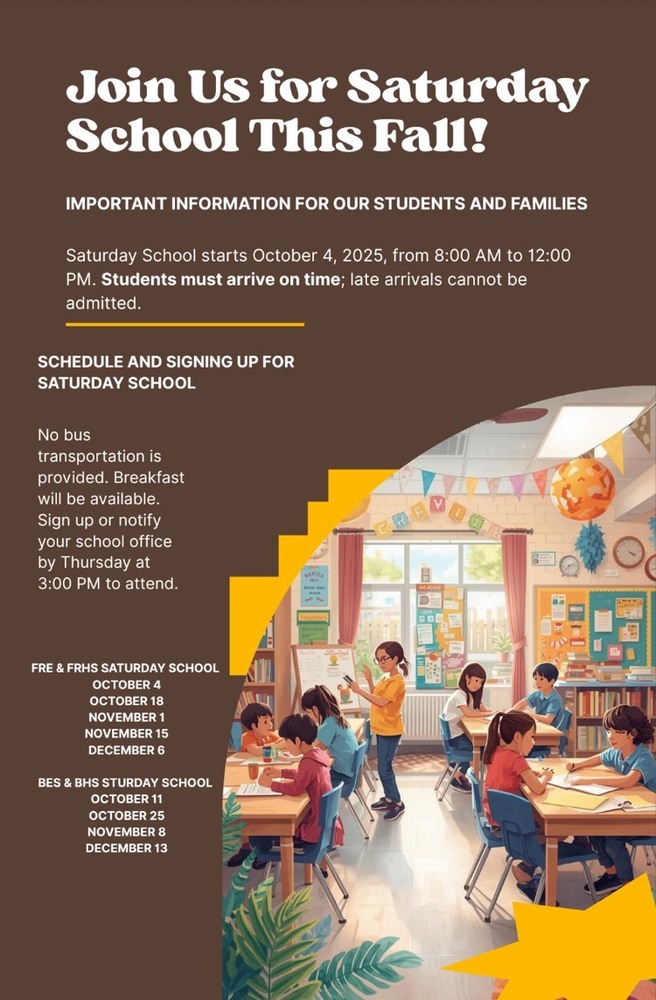
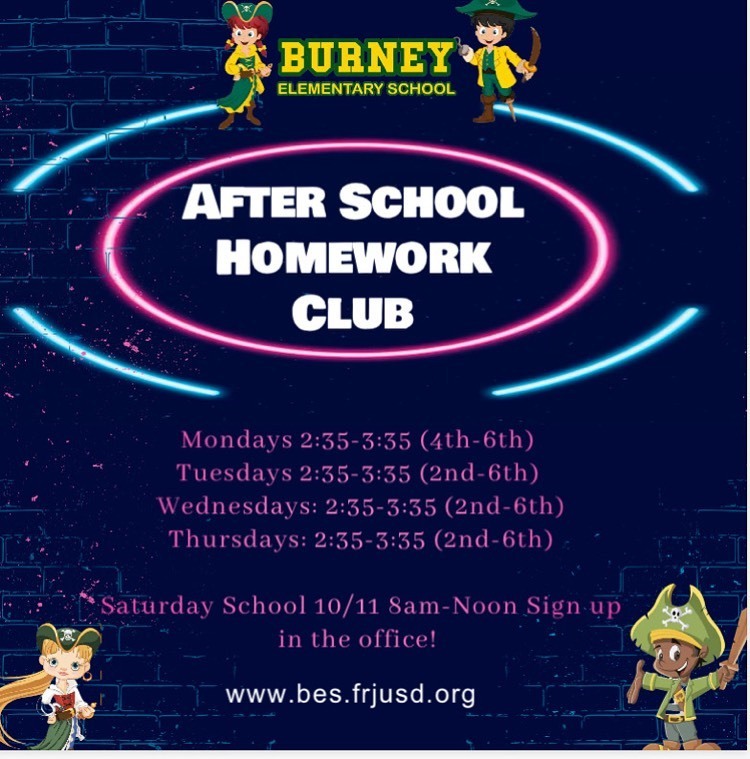
First Saturday School for attendance recovery~ 10/11 8am-12pm ! Sign up in the office! We are excited to share with you a new opportunity for students to improve their attendanc...
September 27, 2025
First Saturday School for attendance recovery~ 10/11 8am-12pm! Sign up in the office! We are excited to share with you a new opportunity for students to improve their attenda...

September 13, 2025
🇺🇸🇺🇸🇺🇸🇺🇸🇺🇸🇺🇸🇺🇸🇺🇸🇺🇸🇺🇸 Patriot Day~ Full School Flag Salute. Thank you Chris Casella Knoch and Board Trustee Megan Estes for attending.
August 12, 2025
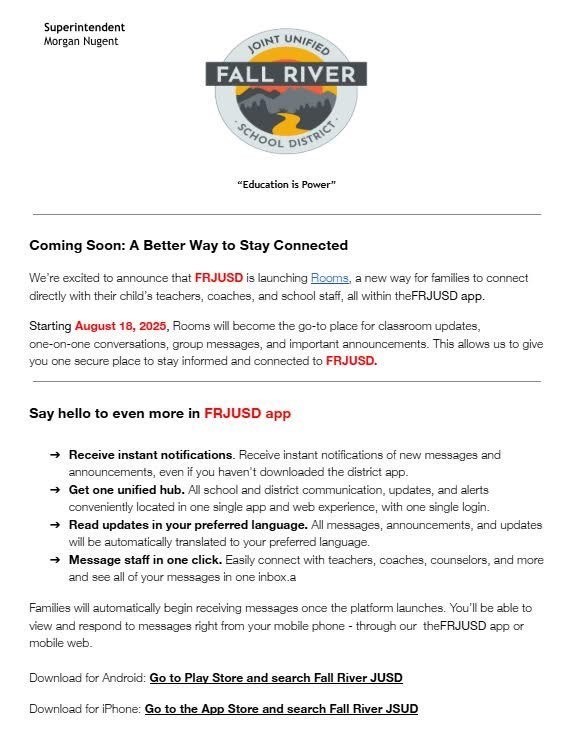
We’re excited to announce that FRJUSD is launching Rooms, a new way for families to connect directly with their child’s teachers, coaches, and school staff, all within the FRJUSD ...
August 1, 2025
Game On! Dear Junior Raider Families, I am so incredibly proud to be part of this amazing community! Our first day is Monday, August 18th - Game On! As we start our new s...
July 14, 2025
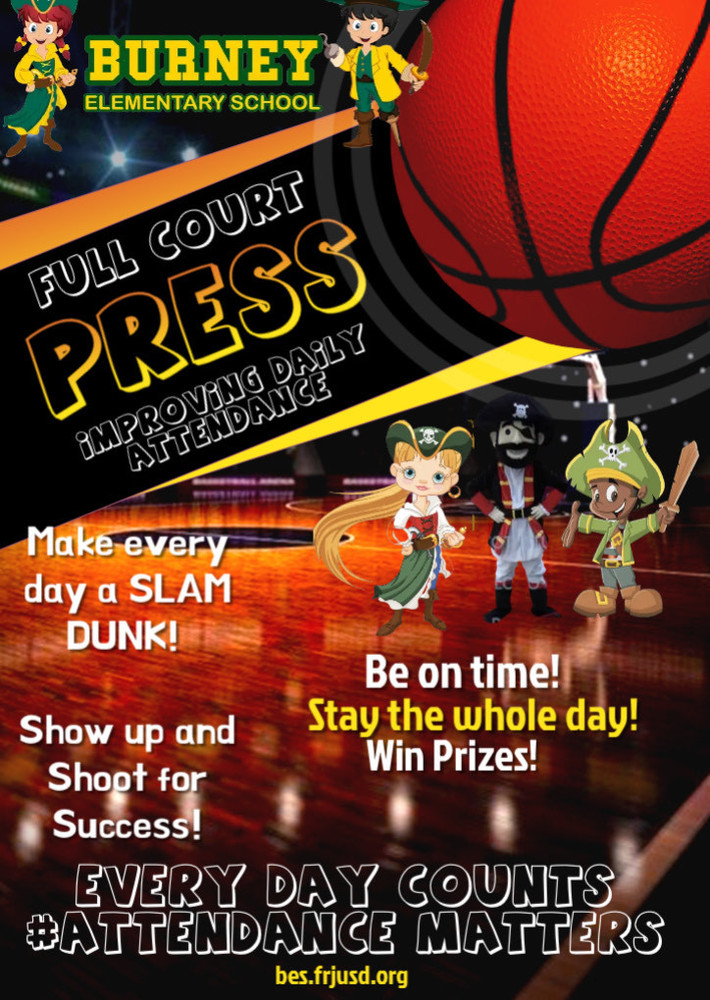
Jr. Raider Families ~ Burney Elementary is taking a full court press approach to boosting attendance, making sure every student is in the game and ready to score big this year! ...

June 14, 2025
Burney Families~ We are Now Enrolling for next school year! Our school office is closed for the summer, but you can enroll at our District Office located at 20375 Tamarack Avenue ...


June 7, 2025
Dear TK Families, As we prepare for the upcoming school year, we wanted to inform you that the dismissal time for TK and Kindergarten students will be 1:15PM. Research and exper...

May 27, 2025
Please fill out this important survey: https://www.surveymonkey.com/mp/take-a-tour/